MANAGEMENT OF OCULAR DISEASES
Millions of patients are diagnosed with diseases and conditions of the eye every year.
Some of which may not display symptoms until there is irreversible damage to the patient’s vision. The outcome of eye disease can range from temporary discomfort to total loss of vision, which is why all eye problems and diseases should be taken seriously and regular eye check-ups are absolutely essential.
What Are The Causes Of Eye Disease?
The main causes of eye problems can be divided into five groups:
- Inflammation of the eye and surrounding structures caused by a bacterial, viral, parasitic or fungal infection.
- Injuries to the eye and surrounding structures, either as a result of trauma or an object in the eye.
- Genetically inherited eye diseases, many of which may only manifest later in life and affect the structures and the functioning of the eye which therefore can impair visual abilities. In some cases, however, children are born with these conditions.
- Diseases or conditions, such as migraine or diabetes, which can affect other organs of the body, such as the eyes.
- External causes, such as allergies or eye strain due to over-use, or as a side effect of medication.
What Are The Symptoms Of Eye Disease?
The three symptoms indicative of eye disease are the change in vision, changes in the appearance of the eye, or an abnormal sensation or pain in the eye.
Changes in vision can include the following symptoms:
- Nearsightedness is caused by an elongation of the eyeball over time, making it difficult to clearly see objects far away.
- Farsightedness is caused by the shortening of the eyeball, making it difficult to see objects that are close-by clearly.
- Blurry or hazy vision, or loss of specific areas of vision, which can affect one or both eyes and is the most common vision symptom. Any sudden changes in vision should be a cause of concern.
- Double vision means a single clear image appears to repeat itself. This could be accompanied by other symptoms like headaches, nausea, a droopy eyelid, and misalignment of the eyes.
- Floaters are specks or strands that seem to float across the field of vision. These are shadows cast by cells inside the clear fluid that fills the eye. These are usually harmless, but should be checked out as they could point to something serious such as retinal detachment.
- Loss of vision after being able to see before.
- Night blindness is the inability to see clearly in the dark or adapting to the dark, especially after coming out of a brightly lit environment.
- Impaired depth perception means a person has difficulty distinguishing which of two objects is closer to him/her.
Changes in the appearance of the eye include, but are not restricted to, the following:
- Redness or swelling of the eyes, which have a bloodshot appearance.
- Watery and itchy eyes, depending on the cause, discharge from the eyes is also possible.
- Redness and swelling of the eyelid.
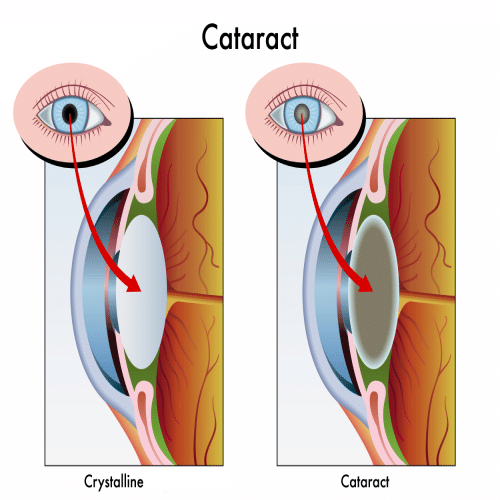
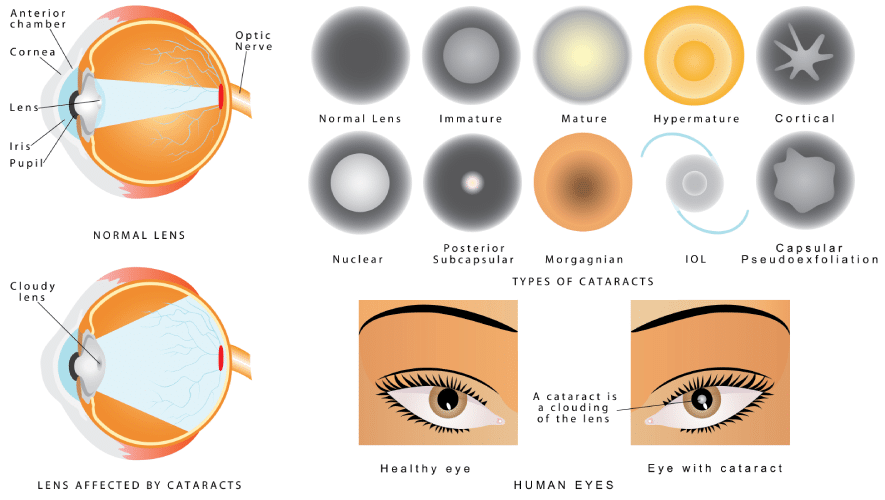
- Cloudy appearance of the eye, which occurs due to a build-up of proteins making the lens of the eye appear cloudy. These can be symptomatic of cataracts.
- Eyelid twitch. This happens when eyelid muscles spasm involuntarily over a period of time.
- Squint
- Bulging eyes could be a symptom of hyperthyroidism or an autoimmune disorder called Grave’s disease.
- Drooping eyelids can be a sign of exhaustion, aging, migraines or a more serious medical problem.
Pain In And Around The Eye

Pain in the eye is called ocular pain, while pain on the surface of the eye is called orbital pain.
Ocular pain can be caused by a scratch or a slight injury to the cornea of the eye or the presence of a foreign object in the eye and often causes redness of the eye. Orbital pain can be sharp or throbbing and may go beyond the surface. This should be a cause for concern if it’s accompanied by vision loss, vomiting, fever, muscle aches, eye-bulging and difficulty in moving the eye in certain directions. Trauma to the eye or the surrounding facial areas can also be the cause of pain.
How Can Eye Diseases Be Treated?
The treatment of eye diseases are divided into four main categories:
- Medication
- Surgery
- Prescription glasses or contact lenses
- Treatment of systemic conditions affecting the eye
Cataracts
If you’ve been diagnosed with cataracts, you may wonder if cataract surgery is right around the corner. Not to worry. There are many preventive steps you can take to slow the progression of cataracts and preserve your vision. That doesn’t mean you won’t eventually need surgery, but you can at least delay the need for quite a while.
Protect Your Eyes From The Sun
The National Eye Institute recommends protecting your eyes from the sun’s harmful ultraviolet (UV) and high-energy visible (HEV) rays by always wearing good quality sunglasses while outdoors. Look for sunglasses that block 100 percent of UV rays and absorb most HEV rays with large lenses or a close-fitting wraparound style. Remember that the peak hours for sun exposure are between 10 am and 3 pm or 11 am and 4 pm during daylight savings time and that the sun’s rays are strong enough to pass through clouds, so you need your sunglasses every day.
Avoid Steroid Eye Drops
Steroid eye drops are routinely prescribed to treat dry eyes or an arthritic flare-up in the eyes. Unfortunately, they can also speed up the progression of cataracts. Talk to your Optometrist about how you can manage both conditions without inadvertently making your cataracts worse – and hastening the need for surgery.
Check Your Medications
There are over 300 commonly prescribed medications with side effects that may impact cataract progression. Since your primary care physician may not have access to your eye doctor’s medical records, be sure to ask your doctor if your current medications will affect your cataracts. If you must stay on the medication, it’s even more important to avoid sunlight during peak hours and to wear sunglasses.
Quit Smoking
If you haven’t quit already, here’s another good reason to do it: over time, the damage from smoking can double or triple an individual’s risk of developing cataracts. If you’ve been a smoker, your habit was probably a big contributor to the diagnosis. The good news is – by quitting smoking now, you can slow the progression of cataracts.
Follow Eye Health Diet Guidelines
Studies have shown that certain vitamins and nutrients may reduce age-related decline in eye health, particularly antioxidants. If you’ve already been diagnosed with cataracts, adding foods rich in antioxidants to your diet will help slow the progression. This list isn’t exhaustive, but here are some examples to get you started: dark chocolate, blueberries, strawberries, pecans, carrots, sweet potatoes, artichokes, kale, red cabbage, beans, beets, spinach, apples, and plums.
Doctors also recommend eating more fish high in omega-3 fatty acids. This has been linked to a potentially reduced risk of cataracts or their progression. You may also consider taking a multivitamin that contains Vitamin C and E. Talk to your doctor or nutritionist about how you might adopt a healthy eating plan that’s designed to prevent cataracts.
Fortunately, making these healthy modifications to your diet can prevent many other lifestyle diseases such as diabetes. Studies have shown that a diet rich in processed carbohydrates can increase your risk of both developing cataracts and speeding up its progression. It’s important to develop a plan that works for you and supports your holistic health.
Take control of your cataract diagnosis by getting regular eye exams, communicating with your doctor, and putting these tips into practice. You’ll have better vision and prevent the need for cataract surgery in the near future.
Can Diet Reverse Diabetic Retinopathy?
Eye disease that is caused by diabetes is currently the number one cause of blindness and vision loss. Due to the increased risk in diabetic patients, doctors recommend that people over 30 with diabetes get an annual dilated eye exam. Diabetic patients under 30 should get this exam five years after they have been diagnosed.
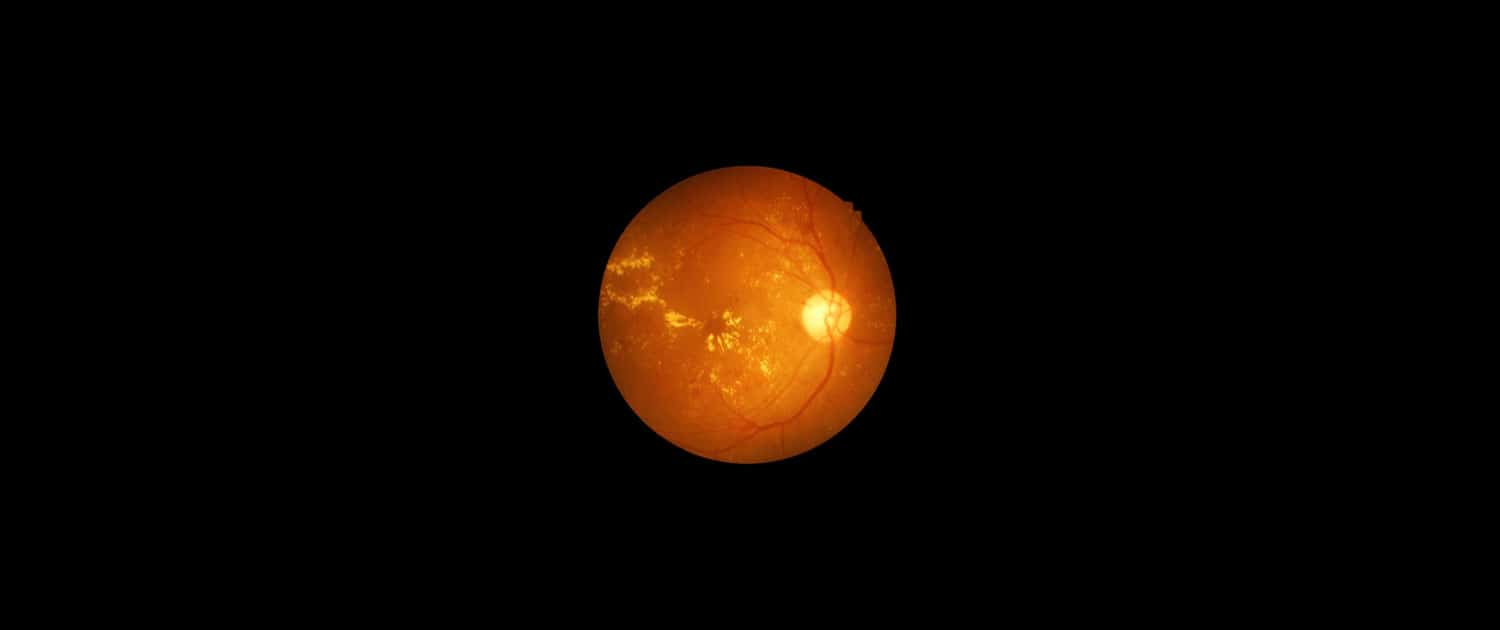
Diabetic retinopathy is a condition that is caused by damage to the retina. Patients that have diabetes may also have experienced extended periods of time where their blood sugar was elevated. The high levels of blood sugar damage the retina’s walls which leave them susceptible to leaking. When fluid accumulates in the retina or macula, it causes vision loss.
To make these matters worse, if prolonged high blood sugar levels are seen again, the retina will be oxygen-depleted. This causes the abnormal growth of new blood vessels. This condition is called neovascularization. This blood vessel type is weak and prone to leaking. As these blood vessels leak, they introduce blood into the eye. Excessive bleeding into the eye can cause blindness.
Treatment
While a healthy diet and exercise can be beneficial to your optical health, diabetic retinopathy is a condition that is caused by damage to the retinal wall. While this damage can sometimes be corrected, simple diet changes won’t reverse the effects.
It is essential to catch the condition in the earlier stages to reduce the effects. This can also help patients understand the importance of monitoring their blood sugar so that repeat events can be limited. Treatment options are even more successful when diabetic retinopathy is caught early. These options include vitrectomy, scatter photocoagulation and focal photocoagulation.
During both scatter, and focal photocoagulation ophthalmologists will use lasers to help alleviate the condition. The lasers make small burns on the retina aimed at the blood vessels. These burns will help to seal the blood vessels to prevent more leakage and stop them from growing larger.
When using scatter photocoagulation, hundreds of small burns are made in a specific pattern during two additional appointments. Scatter coagulation should be used on patients who do not have advanced diabetic retinopathy.
Focal photocoagulation specifically targets the leaking blood vessels that are in the macula. Unfortunately, this procedure is not aimed to correct the blurry vision associated with diabetic retinopathy, but it does stop it from progressing further. Once the retina has detached, neither form of photocoagulation can be used.
Vitrectomy is a surgery that helps to remove scar tissue and/or the fluid that is clouded with blood that has been leaked into the eye. This operation is the most successful when performed before the disease has progressed too far. When the operation only targets removing the fluid, success rates are very high for the procedure. When the procedure also aims to reattach the retina, the failure rate is around 50%.
Living With Retinopathy
Retinopathy affects every person and even the same pair of eyes differently. A one size fits all approach isn’t possible, and it is important to talk to your medical professional about which options or treatment plans are right for you.
It’s important to continue to learn about how you can manage diabetes to help keep the progression of diabetic retinopathy at bay. Make sure to use the tools that are available to you. Test your blood glucose daily, schedule your regular doctor appointments and annual exams, and learn to listen to your body. We can often start to detect that something is going on when things just don’t feel right.
Managing your diabetes with a complete health plan can lead to an increase in the quality of life and help to stop further vision loss.